It often starts with fatigue.
There’s a noticeable increase in thirst and hunger. Vision becomes blurred. Sores are slow to heal, and infections become much more common.
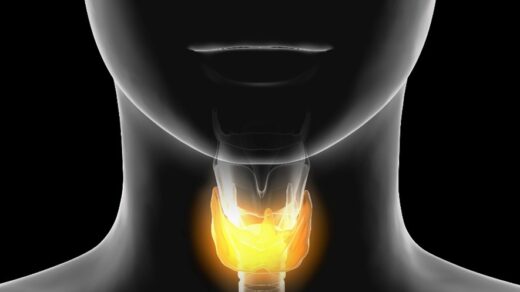
Then there’s the inflammation. And Dr. John Heary says that commonly with type 2 diabetes, it’s internal. Since inflammation was first linked to diabetes, the extent of its role in chronic disease is still being studied. Inflammation also plays a prominent role in thyroiditis, when the thyroid gland becomes significantly swollen.
Inflammation in these two commonly associated disorders is often difficult to manage and can become quickly debilitating — but it can be treated effectively. Here’s how.
Type 2 Diabetes and Thyroiditis Explained
Of the over 37 million people in the U.S. who have diabetes, upwards of 95% have type 2.
With type 2 diabetes, the level of insulin one’s body needs to not effectively produced or the body doesn’t adequately use insulin, a hormone that controls the level of sugar in one’s blood. Insulin is created by pancreatic cells.
Often insulin has an impact on the body’s tissue, especially if one is considered obese. That’s because fat cells are capable of creating the type of chemicals that may lead to inflammation.
In thyroiditis, abnormally low or high levels of thyroid hormones lead to the thyroid gland information. Just as the pancreas plays a vital role in creating insulin, the neck’s thyroid gland is responsible for controlling metabolism and how the body grows.
About 20 million Americans have a form of thyroid disease, and 60% of those are not aware they have the condition.
Inflammation’s Role in Type 2 Diabetes and Thyroiditis
Inflammation is a key driver and symptom of both type 2 diabetes and thyroiditis. Researchers have long focused on the inflammatory pathways that often lead to type 1 and 2 diabetes. In fact, most evidence shows that the course of type 2 diabetes is fundamentally dictated by pathways of inflammation.
The different forms of thyroiditis all feature inflammation to some degree. For example, with Hashimoto’s thyroiditis, one’s immune system damages the thyroid gland leading to swelling. Types of viral infections lead to gland inflammation in De Quervain’s thyroiditis.
In general, thyroid disease is commonly associated with different diabetes forms.

Treatment Options Target Inflammation
Treatment plans targeting type 2 diabetes and thyroiditis often center on controlling resulting inflammation that quickly turns chronic. Since many cases of type 2 diabetes feature inflammation as the direct result of obesity, focusing on nutrition is often key.
Antioxidants and other nutrients that are anti-inflammatory, including a range of vegetables, fruits, and fish are integrated into diets.
Depending on family history, medications such as pioglitazone and liraglutide may be used to control both conditions. With type 2 diabetes, the first essential step is usually finding a medication to manage the resistance to insulin, but diet and exercise also play a strong part.
With thyroid conditions, hormone therapy is typically used with the gland is underactive and medications are more common with overactive thyroid glands. Other options include radioactive therapy and surgery.
The key to treating both type 2 diabetes and hypothyroid is to find the underlying root causes of the disease. Once you find out the underlying cause then you can put an effective plan into place in order to reverse the condition through lifestyle changes, nutrition, diet, and supplements.